Curiethérapie
Curiethérapie
Le mot grec brachys signifie « court ». Ainsi, la « brachythérapie » ou « curiethérapie » désigne une radiothérapie pratiquée à courte distance, contrairement à la « téléthérapie », souvent désignée par l’expression « radiothérapie externe ». La curiethérapie est une forme de radiothérapie interne. Dans ce traitement, on administre une substance radioactive (radio-isotope) directement dans la tumeur, notamment dans une prostate cancéreuse. La radiation détruit les cellules cancéreuses avec le temps.
L’administration de la curiethérapie se fait de deux façons:
La curiethérapie à bas débit de dose ou permanente:
dans ce cas, la dose de radioactivité est très faible, mais permanente. Les implants permanents, comme les grains radioactifs, ne sont pas enlevés. Ils libèrent leur dose de radiation pendant quelques semaines ou quelques mois.
La curiethérapie à haut débit de dose ou temporaire:
dans ce cas, l’on insère temporairement une substance radioactive très forte directement dans la prostate à l’aide de cathéters connectés à une source de rayonnement. On enlève les implants temporaires une fois que la dose de radiation désirée a été administrée.
La curiethérapie à bas débit de dose est principalement utilisée pour le cancer de la prostate à risque faible ou à risque intermédiaire correspondants à des critères médicaux précis. On peut associer la radiothérapie externe à la curiethérapie à haut débit de dose dans le cas du cancer de prostate à risque élevé de progression.
Les matières radioactives les plus fréquemment employées en curiethérapie pour le traitement du cancer de la prostate sont l’iode, l’iridium et le césium.
Le temps nécessaire pour que la radioactivité d’une substance diminue de moitié porte le nom de demi-vie. Les diverses matières radioactives ont différentes demi-vies. Cette information aide l’équipe de radiothérapie à choisir le type de matière à employer et à planifier le protocole de traitement. Cela permet aussi de déterminer pendant combien de temps il faut suivre des mesures de sécurité à la suite du traitement.
Est-ce pour vous
La curiethérapie à bas débit de dose ou permanente
La curiethérapie à bas débit de dose (BDD) ou permanente, souvent appelée par son acronyme anglais LDR (Low Dose Rate), administre de très faibles doses de radiation. Elles sont émises à partir de petites sources contenant de l’iode radioactif, appelé « iode 125 »
Ces sources ressemblent à des grains de riz. Elles demeurent dans la prostate pour toujours. Toutefois, leur radioactivité diminue avec le temps. Après 6 mois, 95 % de la radioactivité est partie. La présence des sources ne cause aucun problème à long terme.
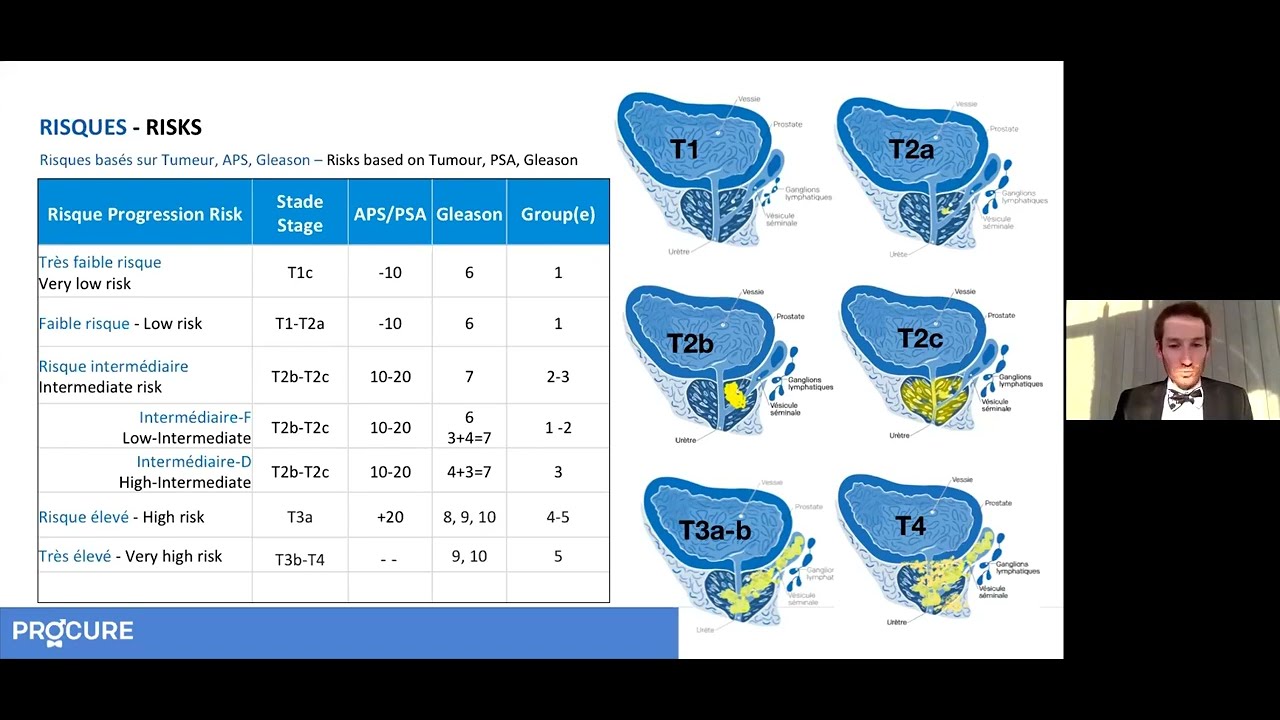
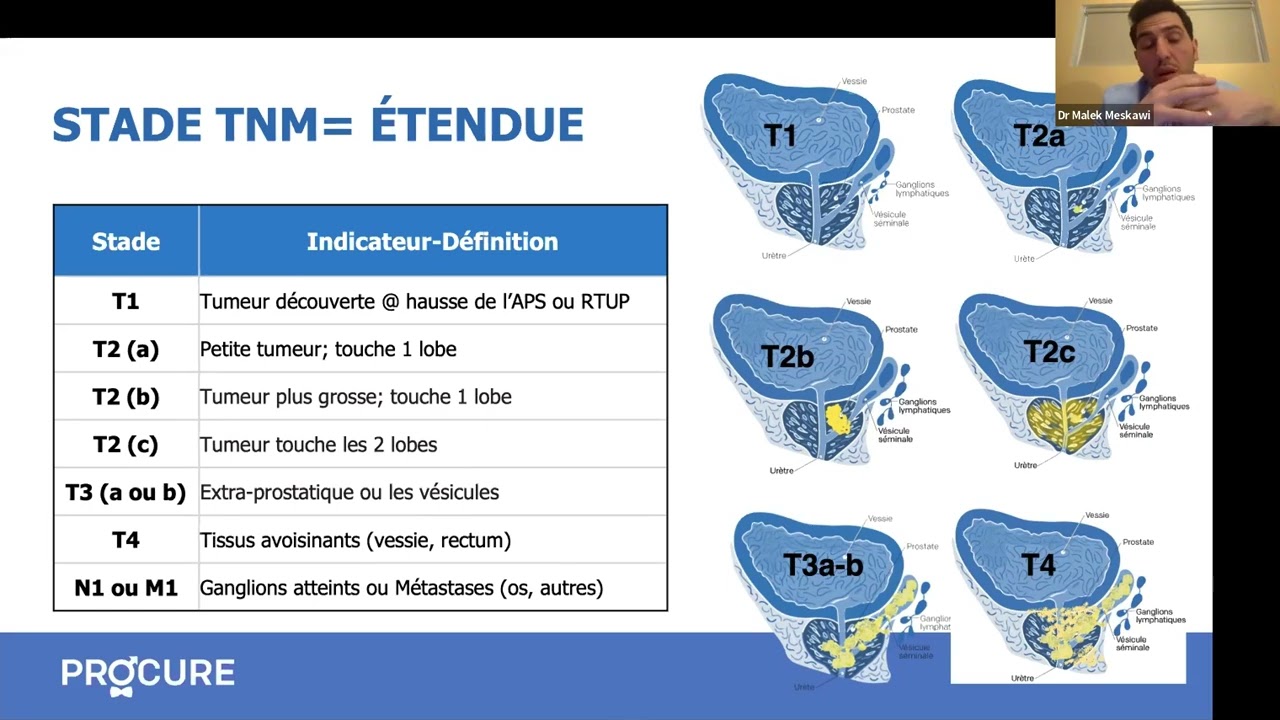
Ce traitement pourrait vous être proposé si vous avez reçu un diagnostic de cancer localisé, de stade relativement précoce (T1, T2a), à croissance lente, donc à faible risque de progression (Gleason 6 ou moins) et avec un taux d’APS bas (en deçà de 10 ng/ml). Elle peut être une option pour des cancers à risque intermédiaires de progression (Gleason 7), mais les patients sont hautement sélectionnés selon des critères précis.
La curiethérapie à haut débit de dose ou temporaire
La curiethérapie à haut débit de dose (HDD) ou temporaire, souvent appelée par son acronyme anglais HDR (High Dose Rate), administre de fortes doses de radiation. Elles sont émises à partir de petites sources contenant de l’iridium radioactif, appelé « iridium 192 ».
Ce type de curiethérapie peut être administré comme un complément d’irradiation ou à titre de traitement unique du cancer de la prostate (monothérapie à forte dose), avec ou sans hormonothérapie.
Utilisée en complément:
de plus en plus, la curiethérapie (HDD) est considérée comme un moyen d’intensification de dose chez tout patient recevant une radiothérapie externe pour le traitement du cancer de la prostate. Elle permet ainsi de réduire le nombre de traitements de radiothérapie conventionnelle. Cette approche est particulièrement utile pour les patients à risque intermédiaire et élevé de progression.
Utilisée en monothérapie:
Bien qu’elle ne soit pas recommandée comme seul traitement pour les hommes atteints d’un cancer de la prostate à risque élevé de progression, elle est de plus en plus utilisée en monothérapie pour les cancers à faible risque ou à risque intermédiaire de progression.
Ce traitement pourrait vous être proposé peu importe les risque de progression de votre cancer (faible, intermédiaire ou élevé).
Considérations additionnelles
La curiethérapie ne peut être recommandée:
- Aux hommes qui présentent des symptômes importants de prostatisme liés à une obstruction urinaire ou qui ont subi une résection transurétrale de la prostate.
- Aux hommes dont le cancer de la prostate s’est métastasé, d’après les scintigraphies osseuses ou les tomodensitométries de l’abdomen et du pelvis.
- Aux homme qui ont subi de radiothérapie pelvienne, qui ont des problèmes de hanches ou qui sont visés par tout autre contre-indication.
Remarques: L’expertise et la technologie étant dispendieuses, ce traitement n’est pas disponible dans tous les centres hospitaliers.
Facteurs justifiant ce choix
Pour de nombreux hommes atteints d’un cancer de la prostate localisé, la curiethérapie offre un traitement efficace sans les risques et les délais de guérison associés à la chirurgie.
Avantages de la curiethérapie
- La récupération est rapide, donc la plupart des hommes peuvent retourner à leurs activités normales peu après le traitement.
- Aucune hospitalisation requise: c’est une intervention d’un jour
- La radiation ne passe pas à travers la peau ou par d’autres organes en santé pour se rendre aux cellules cancéreuses. La curiethérapie cause donc moins de dommages secondaires aux organes voisins.
- Traitement moins exigeant que la radiothérapie traditionnelle et moins éprouvant que la prostatectomie radicale.
- Il n’y a pas de période de convalescence ou de stress opératoire, comme avec la prostatectomie radicale.
Désavantages de la curiethérapie
- Vous aurez généralement besoin d’avoir une anesthésie générale – qui peut avoir des effets secondaires.
- On ne peut connaître exactement la nature et l’étendue de votre tumeur comme après la chirurgie.
- Les échecs ne peuvent que très rarement être traités par voie chirurgicale (l’exception). La radiothérapie peut avoir endommagé la prostate et les tissus environnants, ce qui rend l’ablation de la prostate plus difficile et augmente le risque d’effets secondaires.
- Vous aurez une diminution importante de votre éjaculat et une perte de fertilité si vous voulez des enfants.
- Vous devrez éviter de rester assis très près des femmes enceintes ou des enfants pendant plus de quelques minutes chaque jour, pour les trois premiers mois après le traitement.
Les risques et complications de la curiethérapie
Certains effets indésirables se manifestent immédiatement après l’intervention ou bien quelques semaines plus tard. En général, ils sont temporaires, peuvent durer quelques mois et disparaître progressivement dans l’année qui suit la fin du traitement.
Court-Moyen terme
Les effets secondaires de la curiethérapie sont semblables à ceux de la radiothérapie externe, mais diffèrent un peu. La prostate ayant été percée à plusieurs reprises, ce traitement la fait enfler. Cela peut causer des problèmes urinaires, dont les symptôme peuvent se manifester par:
- des envies fréquentes d’uriner, notamment la nuit
- des envies impérieuses d’uriner (urgence)
- des difficultés à uriner avec un jet moins fort
- des brûlures en urinant
- parfois même un blocage complet des urines (rétention aiguë de l’urine)
De la douleur au niveau du périnée, une présence de sang dans l’urine ou le sperme, des problèmes d’érection transitoires peuvent survenir suite au traitement.
L’irritation des intestins et des troubles rectaux, comme une inflammation du rectum, sont peu courants. Par contre, la diarrhée, une irritation anale, ou des saignements rectaux peuvent survenir dans les mois qui suivent le traitement, quoique très rares.
Long terme
Des effets tardifs peuvent apparaître des mois voire des années à la suite de ce traitement. Les effets secondaires sont variables et peuvent inclure:
- Une dysfonction érectile
- Les risques d’incontinence urinaire ou de symptômes d’obstruction urinaire chronique sont rares (dans les deux cas, moins de 5%).
Ces effets dépendent beaucoup de votre état avant l’intervention. Une personne qui avait déjà de bonnes érections OU peu de problèmes urinaires est moins à risque de conséquences.
Il est important de signaler tout effet secondaire à votre médecin.
Qu’ils soient à court-moyen ou long terme, la plupart peuvent être soulagés par la prise de médicaments ou autres interventions/méthodes.


Votre médecin vous a proposé la curiethérapie pour traiter votre cancer de la prostate? Cette section décrit ce traitement et les précautions à prendre pour que tout se passe le mieux possible. Cliquez ici (ajouter lien) pour mieux comprendre les termes médicaux relatifs à votre appareil reproducteur masculin.
Modalités pour une curiethérapie (BDD)
Durée de l’intervention
L’intervention prend une ou deux heures, mais en comptant la préparation, les calculs et la récupération, il faut parfois compter jusqu’à huit heures.
Installation d’une sonde urinaire
On administre une anesthésie spinale (locale) ou, plus rarement, une anesthésie générale. Une sonde urinaire est mise en place au cours de l’intervention et retirée à la fin. Dans certains cas extrêmement rares, la sonde (ou cathéter) reste en place pendant quelque temps pour faciliter le passage des urines.
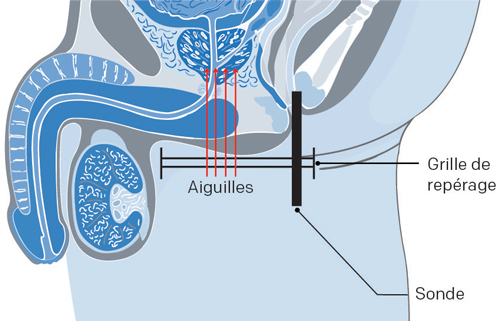
L’intervention
À l’aide de l’échographie transrectale, un spécialiste introduit avec précision les grains dans la prostate aux emplacements prévus. Un radio-oncologue expérimenté implante entre 80 et 100 grains radioactifs dans la prostate.
Repérage des grains
Les grains radioactifs implantés dans la prostate tueront graduellement les cellules cancéreuses au fil des heures et des jours. Une tomodensitométrie spéciale sera pratiquée trois à six semaines après l’intervention pour repérer l’emplacement final des grains et calculer les doses.
Votre taux d’APS
Avec la curiethérapie, on ne s’attend pas à ce que le taux d’APS tombe à 0 ng/mL puisqu’il est pratiquement impossible de détruire 100 % des cellules prostatiques. D’ordinaire, le taux d’APS diminue et se maintient par la suite.
Modalités pour une curiethérapie (HDD)
Durée de l’intervention
L’intervention prend deux à trois heures en salle de traitement et le patient peut quitter en soirée. Dans de rares cas, le médecin peut décider de le garder plus longtemps.
Installation d’une sonde urinaire
On administre une anesthésie générale. Une sonde urinaire est mise en place au cours de l’intervention et retirée à la fin. Dans certains cas extrêmement rares, la sonde (ou cathéter) reste en place pendant quelque temps pour faciliter le passage des urines.
L’intervention
Le médecin entre des petits tubes de plastique vides (de 12 à 18 cathéters ou même plus) dans la peau, entre le scrotum et l’anus. Ces tubes sont ensuite insérés plus creux dans le corps, jusqu’à la prostate à l’aide d’une sonde. Les tubes sont branchés à un appareil de traitement. Cet appareil envoie une source radioactive (Iridium 192) par les tubes. Le traitement dure de 20 à 30 minutes.
Votre taux d’APS
Avec la curiethérapie, on ne s’attend pas à ce que le taux d’APS tombe à 0 ng/mL puisqu’il est pratiquement impossible de détruire 100 % des cellules prostatiques. D’ordinaire, le taux d’APS diminue et se maintient par la suite.
En monothérapie
En cas de monothérapie à forte dose, le traitement est de une à 2 doses en chirurgie d’un jour. Le patient est hospitalisé pendant le traitement. Aucune radioactivité n’est émise quand les cathéters ne sont pas reliés à l’appareil et le patient peut se reposer au service d’urologie générale, entre les interventions, sans devoir être isolé.
Préparation avant la curiethérapie
Une bonne préparation peut rendre la période de récupération après la curiethérapie moins difficile que prévu. Votre préparation jouera un rôle essentiel dans un rétablissement plus rapide et moins stressant. En lisant ce qui suit sur cette page. vous saurez à quoi vous attendre et comment y faire face.
Questions à mon médecin
Nous vous invitons à consulter notre page Questions à poser à votre médecin et votre équipe de professionnels de la santé concernant la curiethérapie. Poser des questions ouvrira la communication, fournira des informations adaptées à votre situation et diminuera le stress lié à la compréhension de ce traitement.
Avant le début du traitement
Peu de temps avant de commencer votre traitement, vous rencontrerez votre équipe médicale dans le but de vous préparer pour votre traitement puis de commencer celui-ci.
Quelques semaines avant le traitement
Vous pourriez recevoir un appel pour avoir un rendez-vous dans une clinique de préadmission. Vous passerez alors divers examens pour compléter votre bilan de santé.
La veille du traitement
Vous ne devez ni boire ni manger à partir de minuit. Si vous devez prendre un médicament, vous pouvez prendre un peu d’eau. Vous devrez vous faire un lavement du rectum, comme on vous l’a expliqué.
Le jour du traitement
lnformez le médecin de tous les médicaments que vous prenez habituellement. Apportez-les dans leur contenant d’origine. Un antibiotique vous sera donné par perfusion avant la procédure.
Apportez à l’hôpital un caleçon pas trop serre, dans lequel vous êtes bien, et une protection absorbante. Vous serez plus confortable lorsque vous retournerez à la maison.
Le déroulement de ces interventions
Le déroulement d’une curiethérapie permanente (avec grains) et celle temporaire diffère selon le traitement. Pour en apprendre davantage sur le déroulement de ces interventions, cliquez ici
La convalescence suite à une curiethérapie
La curiethérapie à haut débit: votre retour à la maison et consignes à suivre sont similaires à ceux décrits pour un traitement de radiothérapie externe.
La curiethérapie à bas débit ne demande qu’une courte période de convalescence.
Pour en savoir davantage sur les inconforts après votre traitement, les mesure de sécurité et la reprise de vos activités sexuelles, cliquez ici
Le suivi médical
Certificat médical
Si vous avez besoin d’un certificat médical, n’oubliez pas de le demander directement à votre radio-oncologue.
Taux de réussite
Comme pour la prostatectomie radicale, il est impossible d’établir un taux de réussite général avec la curiethérapie.
- Cela varie en fonction de chaque cas parce qu’il faut tenir compte du grade diagnostiqué de la tumeur, de son stade de dissémination et du taux d’APS avant le traitement.
- Moins ces données sont élevées, meilleures sont les chances que le patient soit définitivement tiré d’affaire.
Test de l’APS
Le toucher rectal et le dosage de l’antigène prostatique spécifique (APS), effectués régulièrement – tous les trois à six mois – permettent à votre radio-oncologue de surveiller votre état. C’est le test de l’APS qui prédit le mieux le risque de récidive du cancer de la prostate.
Votre taux d’APS
Avec la curiethérapie, on ne s’attend pas à ce que le taux d’APS tombe à 0 ng/mL puisqu’il subsiste toujours des cellules prostatiques normales. D’ordinaire, le taux d’APS descend jusqu’à un plateau et s’y maintient. Votre taux devrait commencer à diminuer dans les mois qui suivent le début du traitement. Il arrive même que votre taux continue de baisser un an après le traitement.
À chaque rendez-vous de suivi, votre radio-oncologue évaluera trois paramètres:
- si le taux d’APS augmente
- combien de temps après le traitement cela s’est-il produit
- et combien de temps faut-il à ce taux pour doubler (c’est sa vélocité)
Récidive
Si le taux d’APS se met à monter, le médecin surveillera combien de temps il lui faut pour doubler. Plus ces périodes sont courtes, plus le risque de récidive est grand et plus cette récidive sera agressive. Par exemple, un taux d’APS qui recommence à monter huit mois après la fin des traitements et qui double en six mois est beaucoup plus inquiétant qu’un taux d’APS qui commence à grimper trois ans après cette intervention et qui met un an à doubler.
Le cas échéant, l’hormonothérapie pourra être prescrite. Sinon, discutez avec votre radio-oncologue des traitements de rattrapage après une curiethérapie.
Rémission
Vous serez suivi pendant au moins cinq ans après votre radiothérapie. Après sept à dix ans sans récidive, les risques que le cancer revienne sont alors faibles.
Les effets secondaires
Les effets indésirables d’une curiethérapie dépendent notamment des éléments suivants :
- le type d’implants (temporaires ou permanents)
- le volume de la région traitée
- la dose d’irradiation ayant pu atteindre les organes voisins, habituellement très faible
- la dose totale reçue
Certains effets indésirables se manifestent immédiatement après l’intervention ou bien quelques semaines plus tard. En général, ils sont temporaires. D’autres apparaissent bien après l’intervention et peuvent durer longtemps. Les problèmes les plus courants associés à la curiethérapie sont les problèmes sur les fonctions urinaires, gastro-intestinales et érectiles.
Fonction intestinale et urinaire
Il arrive parfois que les fonctions intestinale et urinaire prennent plus de temps à revenir à la normale à la fin du traitement.
- Certains médicaments – comme des suppositoires ou des lavements à la cortisone qui permettant de réduire l’inflammation du rectum – et des relaxants musculaires pouvant parfois soulager – peuvent être prescrits.
- Demander un rendez-vous avec une nutritionniste ou une diététicienne pour vos problèmes intestinaux.
- Discutez de vos problèmes urinaires avec votre médecin. Souvent, ils peuvent être facilement corrigés avec un médicament ou une intervention.
Pour en savoir davantage sur les troubles urinaires et intestinaux, consultez notre section sur les effets secondaires.
Fonction érectile
Le pourcentage de risque de dysfonction érectile peut varier selon chaque patient. Cependant, contrairement aux autres effets secondaires, le trouble de l’érection apparaît progressivement plusieurs mois, voire des années après le traitement, mais n’affecte pas la jouissance.
- Comme la mort des cellules est progressive, vous conserverez votre capacité d’érection plusieurs années, mais celle-ci diminuera avec le temps
- Votre capacité érectile dépend de votre fonction sexuelle avant votre traitement, votre l’âge, votre état de santé général.
Pour en savoir davantage sur la dysfonction érectile, consultez notre section sur les troubles sexuels.
Informations complémentaires – Options de traitements
Choix de traitement: Perspective d’un patient et de son médecin
Comment arrête-t-on un choix de traitement pour un cancer localisé?

Le suivi médical après votre prise en charge
Suivez-vous un traitement pour le cancer de la prostate? Diverses approches permettent de le surveiller.
Problèmes urinaires et sexuels après le traitement
Les traitements du cancer de la prostate peuvent entraîner des effets secondaires, comme la dysfonction érectile et l’incontinence urinaire, dont l’intensité et la durée varient.
Tout savoir sur la chirurgie radicale
Envisagez-vous une chirurgie radicale pour votre cancer? Découvrez les détails, avantages et inconvénients dans ce webinaire.
Surveillance, chirurgie ou radiothérapie?
Diagnostic de cancer de la prostate? Plusieurs options de traitement sont disponibles en fonction du stade, de l’âge et de votre état de santé.
La surveillance active comme option de traitement?
Saviez-vous que, dans de nombreux cas, il n’est pas nécessaire de traiter le cancer de la prostate?
Nouveau diagnostic: Comment choisir un traitement?
Plusieurs options de traitement sont disponibles en fonction du stade, de l’âge et de votre état de santé.

Le parcours d’un patient du dx à la rémission
Vous avez reçu un diagnostic de cancer de la prostate? Vous avez des questions sur ce qui vous attend?

Tout sur la chirurgie avec Thierry Dujardin
En quoi consiste cette intervention? Découvrez les détails, avantages et inconvénients dans ce webinaire.

Comment choisir un traitement suite à un dignostic?
Présentation des différentes options par le spécialiste avec témoignages de son patient.

On m’a parlé de fuites, pas d’incontinence
Il n’est pas rare d’avoir des appels de patients nous demandant pourquoi ils souffrent d’incontinence à la suite une chirurgie radicale pour traiter leur cancer de la prostate.

J’ai 4 options de traitement; mêlé vous dites?
Si recevoir un diagnostic de cancer de la prostate est un coup de massue pour les hommes, le choix de traitement peut rapidement donner des maux de tête…

Surveillance active en 5 points
Aussi surprenant que cela puisse paraître, votre médecin peut préférer attendre avant de commencer le traitement.
La curiethérapie permanente: c’est quoi au juste?
La curiethérapie permanente, souvent nommée curiethérapie à bas débit de dose, administre de très faibles doses de radiation. Elles sont émises à partir de petites sources contenant de l’iode radioactif, appelé « iode 125 ». Ces sources d’iode ressemblent à des grains de riz. Elles demeurent dans votre prostate pour toujours. Toutefois, leur radioactivité diminue avec […]

Chirurgie radicale: 5 points à retenir
Si vous avez reçu un diagnostic de cancer de la prostate, votre médecin tiendra compte de nombreux facteurs avant de recommander le meilleur traitement. Pour plusieurs d’entre vous, cela peut signifier enlever complètement la prostate, soit la chirurgie radicale. Voici 5 points à retenir si vous envisagez cette option. La chirurgie radicale, est-ce pour vous? […]
Chirurgie conventionnelle ou robotisée?
Voici un cas typique d’inquiétude de la part d’un patient qui a opté pour la chirurgie radicale comme traitement de son cancer et qui pose cette fameuse question: quelle chirurgie est la meilleure? La chirurgie conventionnelle ou robotisée? Avant d’y répondre, voyons ensemble le contexte dans lequel la question a été posée à nos infirmières […]

Que choisir entre la chirurgie radicale ou la radiothérapie?
À moins de ne pas être candidat pour l’une des deux options, il n’y a en général pas de règles strictes pour décider si la chirurgie radicale ou la radiothérapie est préférable comme traitement. Si votre cancer est vraiment confiné à votre prostate, il peut être guéri par une chirurgie ou une radiothérapie. Cependant, pour […]

Chronologie de récupération après une chirurgie
La chronologie de récupération après une chirurgie radicale de la prostate varie d’une personne à l’autre selon la façon dont leur corps guérit naturellement et la gravité de la maladie avant la chirurgie. Voici quelques conseils pour vous aider dans votre rétablissement. Planifiez votre retour à la maison Après la chirurgie, vous n’aurez pas nécessairement […]

Qu’est-ce qu’une surveillance active réussie
Réussir une surveillance active, est-ce possible? Bien sûr. Est-ce que cela veut dire que votre cancer ne progressera jamais? Non pas du tout. Mais dans 65-70% des cas, le cancer ne progresse pas, car le patient était un bon candidat pour ce type d’option de traitement. Tous les cancers de la prostate se suivent, mais […]
Sources et références
Dernière révision médicale et éditoriale: janvier 2024. Voir notre comité de valiation de nos pages Web et nos collaborateurs en cliquant ici.