All about biopsy
On this page:
Discover our animated video!
Diagnosis and treatment.
Have you recently been diagnosed with prostate cancer? This video is for you! When it comes to cancer, it pays to know the facts. Let’s take a closer look.
Step by step
Prostate biopsy: Everything you need to know
Although the DRE and PSA tests are useful, they are not enough to make a clear diagnosis of prostate cancer. When results are abnormal or questionable, the doctor may order a transrectal ultrasound and a biopsy. These examinations usually provide enough information for a precise diagnosis.
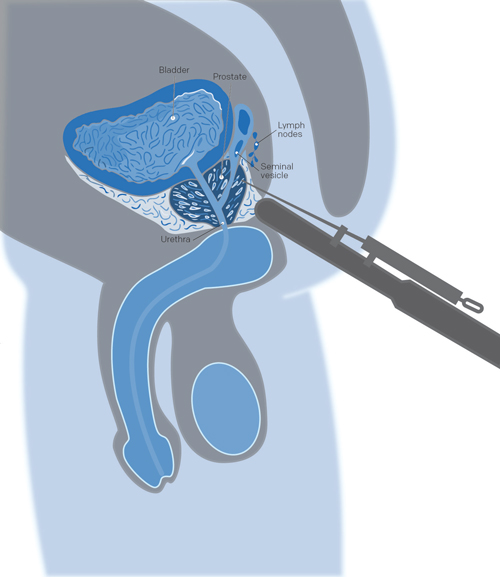
Why
Abnormalities detected during a digital rectal exam and a high PSA level often lead to a prostate biopsy. This procedure consists of taking small tissue samples of your prostate in order for the pathologist to examine them under a microscope to determine if they are cancerous or not. If cancer is detected, the pathologist will use the same samples to calculate your grade (or Gleason Grade Score).
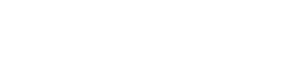
How
A prostate biopsy is usually performed with the help of a transrectal ultrasound (TRUS biopsy). The images taken with the ultrasound help guide a fine needle to the areas selected for sampling. The spring-loaded needle is attached to the ultrasound probe and enters the prostate through the rectum. Usually between 6 – 12 (sometimes more) prostatic tissue samples are obtained and the entire procedure lasts about 10 minutes. A local anesthetic can be used to numb the area and reduce any pain.
Avantages and limitations
Advantages
- A biopsy is the most efficient method of determining if you have cancer and how aggressive it is, that is, how likely it is to spread.
- A biopsy can help you choose the appropriate treatment.
Limitations
- A biopsy can only detect cancer if it is found in the samples taken. It is possible that during sample collection, the biopsy needle could miss the cancerous areas. A normal biopsy result does not completely rule out prostate cancer.
- A biopsy can detect a slow-growing, non-aggressive cancer that might not have caused any problems during your lifetime. In this case, you will need to decide between either undergoing treatment despite the risks or having your cancer monitored.
- A biopsy can have side effects.
Side effects
Bleeding
In the days following a transrectal biopsy, blood may be visible in your excrement. It is possible that you notice reddish or brownish blood in your urine and sperm for several weeks. Light bleeding is normal. However, if it becomes more severe, takes longer to clear up, or if there is a lot of thick-looking, clotted blood in your urine or stools, you should contact your doctor or go to the nearest emergency department.
Pain
In the days following your procedure, you may experience pain or discomfort in the biopsy area. Pain medication can be prescribed if feel that you need them.
Infection
There is a small risk of infection after a biopsy – bacteria on the biopsy needle can get into the prostate. To reduce the risks of infection, antibiotics may be prescribed before and after the procedure. Fever, chills, pain, or burning during urination are signs of infection that can happen even if you are taking antibiotics. If you have these symptoms, contact your doctor or go to the nearest emergency department.
Urine retention
Urine retention is the inability to pee despite having a full bladder. A small percentage of men suffer this side effect following a prostate biopsy. If you suffer from urine retention, speak with your doctor or go to the nearest emergency department.
Results
It takes about two weeks to get the biopsy results because the pathologist needs to examine the samples under a microscope before giving his report.
Presence of cancer
- If the pathologist finds cancer in the samples, he will assess the aggressiveness of the cancer by giving it a Gleason grade.
- You will discuss possible treatments with your urologist who may recommend other complementary tests in order to determine how far your cancer has progressed.
Absence of cancer
- The fact that the pathologist did not find any cancer in your samples can be reassuring. However, it is possible that the biopsy needle simply missed the cancerous areas and you do in fact have cancer.
- If your urologist suspects that you have cancer, he may have you do a second transrectal biopsy or another type of prostate biopsy.
- Otherwise, regular prostate checkups, including the PSA test, digital rectal exam (DRE), and magnetic resonance imaging (MRI), may be the preferred route.
Other types of prostate biopsies
While the transrectal prostate biopsy is the most common, there are other types of biopsies that your urologist may perform.
Transperineal biopsy
Done under local or general anesthesia, this biopsy takes prostate samples by inserting a needle through the skin of the perineum (the region between the scrotum and rectum). As this procedure allows a larger area of tissue to be examined than a transrectal biopsy, your urologist may order one if they think you have cancer despite a negative transrectal biopsy.
Transurethral biopsy
Done under local or general anesthesia, this biopsy goes through the urethra (the tube that runs from the penis to the bladder) to collect the prostate samples. To do this, the urologist inserts a thin tube with a camera attached (a cystoscope) into the penis. A surgical tube is then passed through the cystoscope to collect the samples.
Complementary tests
 If the biopsy confirms the presence of a tumour, additional examinations may be required to determine whether the cancerous cells have spread elsewhere in the body. These are generally undergone by men presenting serious signs of the disease, such as an extensive induration or lump in the prostate, elevated PSA levels or biopsy results indicating the presence of an aggressive cancer. Some of these tests will help the characterization and staging of your cancer.
If the biopsy confirms the presence of a tumour, additional examinations may be required to determine whether the cancerous cells have spread elsewhere in the body. These are generally undergone by men presenting serious signs of the disease, such as an extensive induration or lump in the prostate, elevated PSA levels or biopsy results indicating the presence of an aggressive cancer. Some of these tests will help the characterization and staging of your cancer.
Complete blood count (CBC)
This test, done by taking a blood sample, is not used for staging; it is used to evaluate your overall health by measuring the number and quality of your blood (red blood cells, white blood cells, and platelets). The complete blood count, among other things, checks for infection and anemia that can affect your treatment.
Blood chemistry tests
These tests measure the concentration of various chemical substances in the blood. These chemicals show how well your organs are functioning and can be used to detect damaged tissues or abnormalities. The following chemicals can help stage prostate cancer:
- Urea nitrogen and creatinine. These two substances are normally filtered by the kidneys and excreted in the urine. High levels in the blood mean that your kidneys are either working abnormally or inefficiently. In this case, it is possible that the prostate is blocking urine flow and impairing kidney function.
- Alkaline phosphatase (ALP) and calcium. High levels of these substances may indicate the presence of bone metastases as your cancer spreads to the bone.
Bone scan
Why
A bone scan is an imaging technique used to detect the presence of cancerous cells in the bone where prostate cancer most often spreads. Your urologist will usually order a bone scan if your alkaline phosphatase or calcium levels are elevated or if you have bone pain, or if your urologist has diagnosed you with a more aggressive prostate cancer.
How
A small amount of radioactive material (tracer) is first injected into your blood. You will need to wait two to three hours, the time it takes for the tracers to collect on your bone. During this time, you may need to drink a lot of liquids in preparation for the scan which will last 30 to 45 minutes. During the scan itself, you will lie on an examination table and a camera will take images of your body by moving slowly around you without touching you.
Results
If the images show that the radioactive tracer is spread evenly over all of your bones, your results are normal. However, if prostate cancer has spread to the bones, we usually find it to be concentrated (darker areas) along the spine, ribs, or long bones.
Computed tomography (CT) scan
Why
Computed tomography, often called a CT scan, is also known as a computerized axial tomography (CAT) scan. A CT scan is a form of computed radiography (X-ray) that takes a 3-dimensional image of the internal organs in your body. As prostate cancer often spreads to the pelvic and abdominal nodes, your urologist may be particularly interested in knowing whether the cancer has spread to the smaller organs of your immune system. CT scans can also be used before a radiotherapy treatment to know the prostate’s exact dimensions.
How
For a CT scan, you will probably need to fast for a few hours (no solids or liquids). Before the CT scan, a non-radioactive colorant that helps to see the internal organs more clearly is injected. During the procedure, which lasts about 20 minutes, you will be lying still on a table that will slide slowly into the donut-shaped machine. A camera located on the inside of the machine’s ring will take a series of images of your entire body without ever touching you. You may be asked to hold your breath at times in order to take clearer images. Once completed, computer software will put these pictures together to form a three-dimensional image of the area of interest.
Results
From the images taken, a urologist can see the size and shape of your prostate and determine, among other things, the efficiency of a given treatment. Enlarged lymph nodes could be an indication that they have metastasized and become cancerous. This may affect your course of treatment and other tests may be necessary.
Magnetic resonance imaging (MRI)
Why
Magnetic resonance imaging (MRI), often clearer and more defined than a CT scan, uses magnetic forces and radio-frequency waves rather than X-rays to take a 3-dimensional picture of your internal organs. An MRI lets you see if the prostate cancer has spread to other tissues like the bones, lymph nodes, or seminal vesicles. The MRI can also be used to plan your treatment, to evaluate the efficiency of a treatment, or to follow the cancer’s progression.
How
Before starting the procedure, which takes about an hour, you may be injected with a non-radioactive contrast substance in order to improve image quality. During the MRI, you will lie still on an examination table that slides into a donut- or tunnel-shaped machine. Inform your urologist if you are claustrophobic. Sometimes you may be asked to hold your breath in order to take clearer images. At the end, computer software will put these pictures together to form a three‑dimensional image of the area of interest.
Results
From the images taken, a urologist can see the size and shape of your prostate and determine, among other things, the efficiency of a given treatment. The urologist will also be able to see if the cancer has metastasized out of the prostate which can impact your chosen treatment.
Questions to my doctor
Here is a list of questions about diagnosing prostate cancer for you to ask your doctor and healthcare team.
Read more…
- What test(s) are needed to find cancer? How are they done?
- Will a biopsy be done?
- When will the test(s) be scheduled? Is there a waiting list?
- Who makes the arrangements or appointments for the test(s)?
- Can a support person (such as a partner, parent or friend) be present during the test(s)?
- Where will the test(s) be done?
- Will the procedure be done as an inpatient or outpatient procedure?
- Is an anesthetic or sedation used? If so, what kind?
- Is any preparation needed for the test(s)?
- How long will the test(s) take?
- Are there any side effects to the test(s)? Is the procedure painful?
- Are there any risks involved with the test(s)? What are they?
- Are there special instructions to follow after the test(s)?
- Do I need to arrange a ride home after the test(s)?
- How long does it take to get the results of the test(s)?
- Who will explain the test results?
- May I have a copy of the test results?
- What happens if the results are not normal?
- What other tests will need to be done? Why?
We are here for you
You have questions or concerns? Don’t hesitate. Contact us at 1-855-899-2873 to discuss with one of our nurses specialized in uro-oncology. They are there to listen, support and answer your questions, and those of your family or your loved ones. It’s simple and free, like all of our other services.
Also take the time to visit each of our pages on this website, as well as our YouTube channel, in order to get familiar with the disease, our expert lectures, our section on available resources, the support that is offered to you, our events and ways to get involved to advance the cause.
Staying Informed
Pages that might interest you
Want to know more? Just click on one of the links below.
The latest PROCURE news that might interest
Every week we publish a blog article. Here are some we have chosen for you.
- Prostate cancer: Did you say zero symptoms?
- Scared stiff of having a prostate biopsy?
- Can an MRI of my prostate replace a biopsy?
The medical content and editorial team at PROCURE
Our team is composed of urologists, and nurses certified in uro-oncology with a deep knowledge of prostate cancer and other diseases related to the genitourinary system. Meet our staff by clicking here.
Sources and references
- Prostate Cancer – Understand the disease and its treatments; Fred Saad, MD, FRCSC and Michael McCormack, MD, FRCSC, 4th et 5th editions
- Canadian Cancer Society
- Prostate Cancer Foundation-PCF.org
- National Cancer Institute-USA
- American Cancer Society
- Memorial Sloan Kettering Cancer Center
- Prostate Cancer UK
Last medical and editorial review: September 2023
Written by PROCURE. © All rights reserved