Your diagnosis
Discover our animated video!
Diagnosis and treatment.
Have you recently been diagnosed with prostate cancer? This video is for you! When it comes to cancer, it pays to know the facts. Let’s take a closer look.
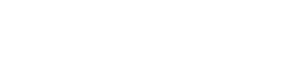
Your Gleason score
The Gleason classification system is the grading system most widely used to describe the degree of aggressiveness of the prostate cancer. Prostatic tissue, obtained by biopsy, is observed under a microscope where a pathologist evaluates the cancerous tissue and compares it to normal prostate tissue. Grading is based on two components: appearance and cellular arrangement. You may have heard talk of the Gleason grade and the Gleason score. Even if the two terms both describe the aggressiveness of cancer, they are not entirely synonyms.
Gleason grade
The pathologist uses a scale from 1 to 5, the Gleason grade, to describe the degree of abnormality in the biopsied tissue samples. The lower the number (grade 1 or 2), the more normal the cancerous cells appear and the weaker the degree of aggressiveness. Inversely, the higher the number (grade 4 or 5), the more the cancerous cells will appear to be irregular or abnormal and the more severe the degree of aggressiveness. A grade 3 is given for an intermediate condition. However, as the prostate is not homogenous throughout the gland, different grades can be assigned within the same tissue.
Low grade
The normal prostate tissue consists of a structured arrangement of ducts and small glands (acini). This is an image of low grade cancer.
Medium grade
As the cancer cells multiply and spread, both the appearance and cellular arrangement will change. The cells change shape and begin to look less like typical prostate cells. This increase in activity also causes the cell nucleus, containing the genetic material for the maintenance, growth and reproduction of each cell, to become larger than normal. All of these changes cause the ducts and glands (acini) of the prostate to take on an irregular appearance.
High Grade
These cancerous cells tend to behave very aggressively, that is to say, they spread quickly. Normal cells die off as they compete against the cancer cells for nutrients. As high-grade cancer cells continue to spread, the ducts and glands (acini) of the prostate also disappear.
Gleason score
The score
In the same tissue, cancer can be more aggressive in some areas than in others (different grades coexist). Thus, to get a more accurate idea of the cancer’s spread, the pathologist assigns grades to the two most common patterns of cancer growth and adds them together to get the Gleason score. It is important to consider the order of the grades. The first number represents the most common grade and can influence your choice of treatment.
The interpretation
For example, the degree of aggressiveness of a cancer with grades 3 + 4 (Gleason score 7) will be lower than a cancer with grades of 4 + 3 (Gleason score 7). In cases where a predominant grade cannot be found, the pathologist will add the number to itself. For example, 4 + 4 gives a score of 8.
The Gleason scale
In theory, the Gleason score is a scale from 2 to 10, but in practice, because grades 1 and 2 are not cancer, scores are normally only between 6 and 10 (3 + 3 to 5 + 5). In general, the higher the score, the more aggressive and fast-growing it is. The Gleason score can be an important factor in your doctor’s recommendation to proceed with a radical prostatectomy.
The new classification system
In recent years, a new classification system has been used to assess the aggressiveness of prostate cancer: Grade Group. It simplifies classification into 5 groups.
Grade Group 1 = Gleason Score 3+3
Grade Group 2 = Gleason Score 3+4
Grade Group 3 = Gleason Score 4+3
Grade Group 4 = Gleason Score 8/10
Grade Group 5 = Gleason Score 9/10 or 10/10
Your clinical stage
Your urologist will analyze all the results of the tests you have done and will give a stage for your cancer depending on the size and spread of the tumour. The most commonly used method for classification is the TNM method (Tumour, Nodes [lymph nodes], and Metastases).
The T refers to the extent of the main (primary) tumor, N for whether the cancer has spread to nearby lymph nodes and M for whether the cancer has spread (metastasized) to other parts of the body.
There are 2 types of T categories for prostate cancer:
- The clinical T category (written as cT) is your doctor’s best estimate of the extent of your disease, based on the results of the physical exam (including a digital rectal exam) and prostate biopsy, and any imaging tests you have had.
- If you have surgery to remove your prostate, your doctors can also determine the pathologic T category (written as pT). The pathologic T is likely to be more accurate than the clinical T, as it is done after all of your prostate has been examined in the lab.
The clinical stages of prostate cancer
T: Size and extent of the tumour
TX – Tumour cannot be assessed.
T0 – Absence of tumour in the prostate.
T1 – Tumour is small, confined to the prostate and cannot be felt during a digital rectal exam. This is a localized prostate cancer.
- T1a – found in 5% or less of tissue removed for another condition (eg, BPH).
- T1b – discovery in more than 5% of tissue removed for another condition (eg BPH).
- T1c – discovered as a result of increased PSA, and prostate biopsy and may be present in one or two lobes.
T2– Tumour is contained to the prostate but can be felt during a digital rectal exam or seen on imaging (MRI). This is a localized prostate cancer.
- T2a – Tumour has spread to half of the prostate lobe or less.
- T2b – Tumour has spread to more than half of only one of the prostate lobes.
- T2c – Tumour has spread to both prostate lobes.
T3 – Tumour has started to spread beyond the prostate to areas surrounding the gland. This is a locally advanced prostate cancer.
- T3a – Tumour has broken through the capsule of the prostate (the anatomical barrier that lines the exterior of the prostate), but has not spread to the seminal vesicles.
- T3b – Tumour has spread to the seminal vesicles.
T4 – Tumour has spread beyond the prostate to nearby structures other than the seminal vesicles: rectum, urethral sphincter, bladder, and pelvic wall. This is a locally advanced prostate cancer.
N: Spread to the nearby lymph nodes (pelvic)
NX – Nearby lymph nodes are not measured.
N0 – No cancer cells in the nearby lymph nodes.
N1 – Cancer cells present in the regional lymph nodes.
M: Spread to distant sites (distant metastases)
MX – No assessment of distant sites or results are inconclusive.
M0 – No distant metastases.
M1 – Distant metastases (bones, non-regional lymph nodes, liver, kidneys, lungs). This is a metastatic prostate cancer.
The Union for International Cancer Control membership organization
The UICC groups the TNM data into four stages:
Stage I
- T1-N0-M0
- T2a-N0-M0
Stage II
- T2b-N0-M0
- T2c-N0-M0
Stage III
- T3-N0-M0
Stage IV
- T1/2/3/4-N1-M0
- T1/2/3/4-N0/1-M1
Stade 1 à 4



Risk of your prostate cancer spreading
Low risk
Your cancer may be at low risk of spreading if:
- Your PSA level is less than 10 ng/mL, or
- Your Gleason score is 6 or less, or
- Your cancer is stage T1 or T2a
Medium risk
Your cancer may be at medium risk of spreading if:
- Your PSA level is between 10 and 20 ng/mL, or
- Your Gleason score is 7, or
- Your cancer is stage T2b
High risk
Your cancer may be at high risk of spreading if:
- Your PSA level is higher than 20 ng/mL, or
- Your Gleason score is 8, 9 or 10, or
- Your cancer is stage T2c, T3 or T4
Your type of cancer
 Localized prostate cancer
Localized prostate cancer
Localized prostate cancer is contained within the prostate, in other words, it has not spread outside of the prostate. Many localized cancers are often not very aggressive and tend to grow slowly. Because of this, chances are high that this type of cancer will not cause you any problems in your lifetime. However, some localized cancers grow more quickly than others and can spread to other parts of your body.
There is no perfect treatment for localized cancer; each treatment has its strengths and weaknesses. A radical prostatectomy (the complete removal of the prostate) or a radiation therapy treatment can be done, but simply keeping a close watch can be enough to find any cancerous growth in time. Discuss the possible courses of treatment with your urologist.
Locally advanced prostate cancer
Locally advanced prostate cancer is cancer that has begun to break out of the prostate, but not too far. It may have spread beyond the boundaries of the prostate (capsule) into the neighbouring regions of the seminal vesicles, pelvic nodes, bladder, rectum, or pelvic lining.
Selecting the best treatment depends on the extent of the cancer spread:
- Radical surgery and pelvic lymph node dissection
- Radical surgery with adjuvant pelvic radiotherapy (after surgery)
- External radiotherapy combined with long-term hormone therapy (18-36 months)
- External radiotherapy combined with temporary brachytherapy
- Hormone therapy alone
Metastatic prostate cancer
Metastatic prostate cancer is cancer that has spread to other parts of your body — far from your prostate. Metastases originating from the prostate most often develop in the bones and lymph nodes. Bone pain, fatigue, and weight loss are all symptoms associated with advanced cancer. Advanced prostate cancer cannot be cured. There are, however, many treatments that can help to reduce symptoms and keep your cancer under control for several years. The preferred treatment for metastatic prostate cancer is hormone therapy, which aims to reduce the level of testosterone (castration), a hormone that nourishes cancer cells. It can be done surgically by removing the testicles or medically by injections or medication.
In recent years, several treatments initially used after the failure of hormone injection, such as chemotherapy and/or next-generation hormone therapy in the form of tablets, are now sometimes used when a new diagnosis of metastatic prostate cancer is made.
What 2023 research says – In patients with prostate cancer that has spread significantly throughout the body, treatment options beyond just hormone injections, such as triple therapy (standard hormone therapy, chemotherapy and oral tablets), should be discussed with your doctor. As such, here is a video clip that might interest you with Dr. Aly-Khan Lalani, Medical Oncologist at the Juravinski Cancer Centre and Assistant Professor at McMaster University, in Ontario, Canada, following the ASCO-GU scientific conference in 2023.
Other types of prostate cancer
Recurrence
The recurrence of cancer can happen when some cancer cells survive after your initial treatment. Cancer can recur in the same place or it can be detected in another part of your body. The latter is also known as a metastatic recurrence. The next treatment step depends on the location of the recurrence.
Castrate resistant prostate cancer (CRPC)
Hormone therapy can keep the spread of cancer under control for a number of years. However, with time, the cancer may become castrate resistant and start to grow again. That is to say, cancer is able to replicate despite castration (the low level of testosterone). Treatments for cancers that no longer respond to hormone therapy exist, but are dependent on whether or not metastases are present.
Rare types of prostate cancer
The majority of men who have prostate cancer are diagnosed with adenocarcinoma, a malignant tumour in the glandular cells lining an organ. However, rare forms of prostate cancer also exist; the following are examples of such:
Sarcoma
Leiomyosarcoma and rhabdomyosarcoma affect, respectively, smooth and striated prostatic muscle cells. These cancers don’t usually affect PSA levels, but often cause urinary problems. Sarcoma is found during biopsy, imaging or following a transurethral resection of the prostate used to treat urinary problems.
Neuroendocrine carcinoma
This cancer develops from neuroendocrine prostate cells. There are “small cell” neuroendocrine cancers and “large cell” neuroendocrine cancers that are much rarer and much less studied. Small cell carcinoma does not usually affect PSA levels and is often found following a biopsy or transurethral resection of the prostate that is used to treat urinary problems. This form of cancer tends to be aggressive, spreading to other parts of the body (metastases).
Transitional cell carcinoma
This cancer can start in the prostate, but more often than not, it starts in cancerous cells lining the urinary system (bladder, urethra, ureter, and kidney) and spreads to the prostate. This cancer is often diagnosed following a transurethral resection of the prostate.
Whether you are diagnosed with a rare form of prostate cancer or another less common type, such as ductal carcinoma, mucinous carcinoma, or signet ring carcinoma, ask your doctor to give you a detailed explanation of the cancer that you are affected by and its possible treatments.
Where can it spread
If my cancer spreads
Places where prostate cancer most commonly spreads
One of the characteristics of cancer cells is their ability to spread to other parts of your body from where they originally started growing. The spread of cancer can happen in three different ways:
- Local invasion: by growing, the tumour spreads into neighbouring tissues.
- Lymphatic spread: cancer cells break away from the tumour, and enter into lymphatic circulation in another regional or remote ganglion.
- Hematogenous spread: cancer cells break away from the tumour, enter into the bloodstream, and start growing in a new location.
For the majority of cancers, places where the cancer usually spreads to are known and predictable. In the case of prostate cancer, cancer cells have a tendency to spread to the following places:
- ureter
- bladder
- urethra
- rectum
- lymph nodes located close to the prostate
- bone, especially the spinal cord, pelvis, femur, and ribs.
- lung (very rare)
- liver (very rare)
- brain (very rare)
Possible emergencies linked to the spread of cancer
The following are a few of the serious consequences that can result from the spread of cancer:
- Ureter obstruction can cause acute renal failure.
- Bladder outlet obstruction can lead to trouble emptying the bladder.
- Brain metastases can cause a variety of symptoms such as headaches and disturbances in mood, speech, movement, and internal bodily functions.
- Spinal cord compression can result in weakness, numbness, or even paralysis of the legs.
We are here for you
You have questions or concerns? Don’t hesitate. Contact us at 1-855-899-2873 to discuss with one of our nurses specialized in uro-oncology. They are there to listen, support and answer your questions, and those of your family or your loved ones. It’s simple and free, like all of our other services.
Also take the time to visit each of our pages on this website, as well as our YouTube channel, in order to get familiar with the disease, our expert lectures, our section on available resources, the support that is offered to you, our events and ways to get involved to advance the cause.
Staying Informed
Pages that might interest you
Want to know more? Just click on one of the links below.
The latest PROCURE news that might interest you
Every week we publish a blog article. Here are some for you.
- Did you say prostate cancer?
- I want to postpone my treatment… Is that wise?
- Prognosis = Doctor, will I be cured?
The medical content and editorial team at PROCURE
Our team is composed of urologists, and nurses certified in uro-oncology with a deep knowledge of prostate cancer and other diseases related to the genitourinary system. Meet our staff by clicking here.
Sources and references
- Prostate Cancer – Understand the disease and its treatments; Fred Saad, MD, FRCSC and Michael McCormack, MD, FRCSC, 4th et 5th editions
- Canadian Cancer Society
- Prostate Cancer Foundation-PCF.org
- National Cancer Institute-USA
- American Cancer Society
- Memorial Sloan Kettering Cancer Center
- Prostate Cancer UK
Last medical and editorial review: April 2023
Written by PROCURE. © All rights reserved