Hormone therapy
Discover our animated video!
The role of hormone therapy.
Has your doctor recommended hormone therapy to treat your prostate cancer? This video is for you! When it comes to hormone therapy, it pays to know the facts. Let’s take a closer look.
Overview
Hormone therapy aims to block the production or effects of hormones, such as testosterone and dihydrotestosterone (DHT), that are produced by the testicles. It is used to slow the growth of cancer or to relieve pain or other symptoms (palliative care).
Why and for whom
Male hormones are called androgens, which include testosterone and DHT, and contribute to the growth of cancer cells in the prostate. Hormone therapy fights prostate cancer by preventing your body from secreting or using hormones which slows the growth and spread of your cancer. Hormone therapy treats your whole body rather than targeting only your prostate.
Hormone therapy may be used:
- as the primary treatment for advanced or recurrent prostate cancer.
- before, during, or after radiation therapy for men who have high-risk prostate cancer and in some men with intermediate-risk cancer.
- to relieve pain or control symptoms of advanced prostate cancer (palliative therapy).
Approaches and modalities used most often
- Intravenous drugs that block the testicles from producing testosterone.
- Drugs taken orally that prevent prostate cancer cells from using testosterone or that reduce the amount of testosterone that prostate cancer can use for growth.
- A surgical procedure involving the removal of the testicles that produce most of the body’s testosterone (to maintain appearances, artificial testicles can be inserted during the procedure).
While these treatments can help to relieve your symptoms, they do not lead to a cure. However, as they affect your entire body, it can help slow the growth of your cancer regardless of which body part the cancer cells have spread to.
Is it for you
 Let’s see
Let’s see
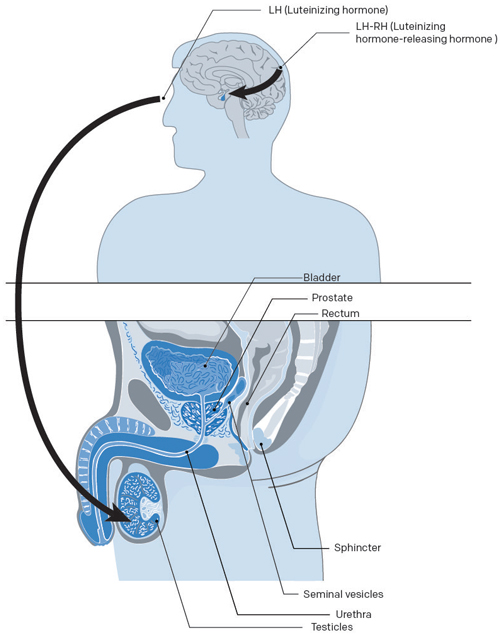
Hormone therapy aims to lower the level of androgens (male hormones) circulating in your body and slow the growth of your prostate cancer by blocking either the production of testosterone or the transmission of signals from your brain that instruct the testicles and adrenal glands (hormone secretion) to produce testosterone.
- Male hormones are called androgens. Testosterone—the hormone responsible for the development of male sexual characteristics—is produced mainly by the testicles and in lesser amounts by the adrenal glands.
- Testosterone stimulates prostate growth. When prostate cancer cells develop, they rely on testosterone for continued growth.
Hormone therapy is used primarily when early treatments, such as radical prostatectomies and radiation therapy, have failed.
Hormone therapy is also useful when a patient is unable to or refuses to undergo surgery or radiation therapy. On occasion, it can be combined with another treatment like radiation therapy.
Who can undergo hormone therapy?
The type of hormone therapy used, the dosage administered, and the treatment plan followed will vary from person to person.
- Men whose cancer has returned following a different treatment, such as radiation therapy or surgery, or men who have a high risk of recurrence after the aforementioned treatments.
- Men whose prostate cancer has spread beyond the prostate and into other parts of the body (stage N1 or M1).
- Men who do not qualify as candidates for surgery, radiation therapy, or brachytherapy.
- Men with advanced cancer can use this treatment as a way to control the cancer and manage cancer symptoms.
Neoadjuvant hormone therapy (before a treatment)
Hormone therapy is sometimes recommended several months before your external beam radiation therapy or brachytherapy treatment. This is done to reduce the size of your tumour which will in turn make it easier to be irradiated. This is called neoadjuvant hormone therapy. Hormone therapy is not recommended before a radical prostatectomy.
Adjuvant hormone therapy (after a treatment)
Adjuvant hormone therapy is given after a radical prostatectomy or radiation therapy. The doctor will resort to this treatment if it is thought—based on your grade, stage, and PSA level—that the cancer has spread to other parts of your body.
This does not mean that your cancer has metastasized, but rather there is a risk of recurrence if isolated cells, which are often undetectable, remain in your body. This treatment takes 4–6 months for an intermediate risk of recurrence and 2–3 years for a high risk of recurrence.
Concomitant hormone therapy (during a treatment)
Concomitant hormone therapy is given during a treatment, such as radiation therapy, for high-risk prostate cancer and in some cases of intermediate-risk cancer.
Intermittent hormone therapy
Hormone therapy is stopped when the PSA rate decreases and stabilizes. It resumes when the APS rate starts to increase, this can take several months and sometimes even years. Intermittent treatment theoretically has the advantage of allowing the patient to regain “normal” sexual activity and to eliminate side effects during periods without medication.
It would be best to talk it over with your doctor.
Reasons for choosing hormone therapy
Hormone therapy can slow prostate cancer growth but cannot cure it. For advanced cancer cases, it is an excellent way to manage pain.
However, the duration and effectiveness of this treatment varies depending on the patient. 70–85% of men who receive this treatment respond for a certain amount of time. For some men, this respite may last more than 10 years; while for others it will last less than a year.
Types of hormone therapies
 Hormone therapy offers numerous possibilities with which to treat prostate cancer. Different molecules and associations exist; if they all acted in the same way (chemical castration), they would not have the same side effects.
Hormone therapy offers numerous possibilities with which to treat prostate cancer. Different molecules and associations exist; if they all acted in the same way (chemical castration), they would not have the same side effects.
The three main types
There are three main types of hormone therapy for prostate cancer:
- Injections or implants to stop you from producing testosterone.
- Tablets to block the effects of testosterone.
- Surgery, called an orchiectomy, to remove your testicles or the part of your testicles that produces testosterone.
The most common hormonal therapies used to treat prostate cancer are:
- Luteinizing hormone-releasing hormone (LHRH) agonists
- Luteinizing hormone-releasing hormone (LHRH) antagonists
- Anti-androgens
- Estrogens
- Surgery to remove the testicles (orchiectomy)
LHRH agonists (or antagonists)
The doctor will administer LHRH agonists or antagonists for hormone therapy before or after your treatment.
These drugs prevent your testicles from producing testosterone which provides your prostate cancer with nourishment. Stopping testosterone production reduces the size of both your tumour and prostate.
How is it administered?
Luteinizing hormone-releasing hormones are given as regular injections. Depending on the drug, injections are given every month or every 3, 4 or 6 months. Depending on the case, this treatment can be given continuously for the rest of life or intermittently depending on how the cancer responds.
The most common LHRH agonists are:
- leuprolide (Lupron, Lupron Depot, Eligard)
- goséréline (Zoladex)
- buséréline (Suprefact)
- triptoréline (Trelstar)
The LHRH antagonist is:
- degarelix (Firmagon)
Anti-androgens
Anti-androgens block the effects of testosterone on your prostate cancer cells. The drug attaches to androgen receptors on prostate cancer cells and prevents them from using the testosterone in your blood stream.
If you are taking LHRH agonists, anti-androgens may be given for a short time in order to reduce pain and symptoms of the tumour flare reaction caused by the agonists.
How is it administered?
Anti-androgens can be taken orally in pill or liquid form.
- Monotherapy
- Before injections or implants
- At the same time as injections or implants
- After surgery to remove the testicles (orchiectomy)
The most common types of anti-androgens are:
Estrogens
Estrogens are female hormones that lower the level of androgens. Estrogens are no longer used because they cause cardiovascular problems.
Orchiectomy
Orchiectomy is a form of hormone therapy that involves surgically removing your testicles. This radical treatment can lower the concentration of testosterone by 90–95%. This procedure, also known as “chemical castration”, is a day surgery performed under local anesthesia.
The advantage of orchiectomy is that the man does not require frequent drug injections. The disadvantage of orchiectomy is that most men may feel that this surgery will make them less masculine.
Advantages and limitations
 Avantages of hormone therapy
Avantages of hormone therapy
- Hormone therapy is an effective treatment for prostate cancer.
- It can treat prostate cancer regardless of where it is in your body.
- It can be used in combination with other treatments to make them more effective.
- It can help reduce certain advanced cancer symptoms such as urinary symptoms and pain associated with metastases.
Limitations of hormone therapy
- It can cause side effects that can have a significant impact on your daily life.
- Some side effects, such as breast augmentation, are permanent.
- Used alone, hormone therapy does not cure cancer—but it can keep it under control, sometimes for several years.
- The duration of side effects differs depending on the patient.
Risks and complications
Hormone therapy drugs have revolutionized patient care for hormone dependent cancers. However treatments, which can last several years, often cause side effects that require additional care and adapted support.
- Side effects can manifest at any point during your hormone therapy treatment. Some side effects occur during treatment while others develop immediately after or a few days or even several weeks later.
- Most side effects will go away once you finish your hormone therapy. Certain side effects can develop months or even years after treatment. Depending on the duration of your treatment, some side effects can last a long time or be permanent.
- It is important to report any side effects to your doctor. Your doctor will grade (measure) how severe the side effects are. If side effects are serious, you may need to adjust your dose.
Short–Medium term
Side effects include:
- Loss of libido (sex drive)
- Erectile dysfunction (inability to have an erection)
- Hot flashes
- Weight gain and muscle loss
- Breast swelling and tenderness
- Fatigue
- Irritability
Long term
Long-term use of more than a year can result in the following side effects:
- Anemia
- Bone thinning (osteoporosis)
- Changes in male characteristics (e.g. shrinking of the testicles)
- Possible increase in risk of cognitive (concentration, memory) or mood (depression) disorders
- Increased risk of cardiovascular disease (heart attack, stroke, etc.)
- Increased risk of developing a metabolic syndrome (diabetes, dyslipidemia, obesity, hypertension, etc.)
Medical follow-up
 Why it is important
Why it is important
The results
Hormone therapy does not cure prostate cancer but controls it, allowing you to live longer and maintain a good quality of life. Each case is different because the diagnosed grade of each person’s tumour, their dissemination stage, and pre-treatment PSA levels will vary.
Your doctor will monitor your progress by conducting a digital rectal examination and PSA screening on a regular basis—every 3-6 months. The faster your PSA level falls, the better your chances are of having your cancer under control.
The objective, however, is to stabilize PSA levels, not to reach 0 ng/mL (although if the patient has also undergone a radical prostatectomy, PSA should be undetectable). As long as PSA levels remain stable, the cancer is considered to be in remission.
Recurrence
At every appointment, a new blood sample is taken so that your doctor can monitor your PSA level. If the PSA level starts to climb, the doctor will monitor how much time it takes to double. The shorter this period is, the greater the risk of recurrence and the more aggressive the recurrence will be. If the cancer recurs, that means it is castration-resistant (formerly called hormone-refractory), and the patient may have to turn to other treatments.
The next article You no longer respond to hormone therapy and don’t have any metastases? will give you an idea of what happens next.
Hope and advances in research
Testimonial of Robert and his son, Jean-Marc Evenat
To see our other testimonials, click here.
Side effects
 No matter what prostate cancer treatment you undergo, there is always the possibility of developing side effects. However, not everyone gets side effects; if you do get side effects, not everyone feels them in the same way. Side effects of hormone therapy are dependent on the following:
No matter what prostate cancer treatment you undergo, there is always the possibility of developing side effects. However, not everyone gets side effects; if you do get side effects, not everyone feels them in the same way. Side effects of hormone therapy are dependent on the following:
- The type of hormone therapy (surgery or drugs)
- Your medication dose and duration (how long you take it for)
- Your overall health
The side effects, although transient, can be difficult to manage, and some patients are tempted to stop treatment. However, it is important to bear in mind the major therapeutic impact of hormone therapy. In addition, there are usually ways to manage them and help the patient overcome them.
Do not hesitate to talk about all of your side effects with your doctor during your follow-up visits.
Loss of libido
The drop in hormone production resulting from surgical or medical castration will lead to a decrease in sexual desire (loss of libido). After more than two years of continuous medication, testosterone levels may never return to normal. Drugs that help you maintain an erection are not very helpful if you don’t have a sex drive. In most cases, your sexual desire will gradually return once you finish your treatments.
What you can do…
- You should consult a professional counsellor or a sex therapist, either alone or with your partner. These professionals can help couples to strengthen emotional ties, communicate, and explore different ways to be intimate. To learn more, we invite you to view our conference on Sexuality and intimacy.
Erectile dysfunction
Erectile dysfunction is a very common side effect of hormone therapy. Whether erectile dysfunction is permanent or temporary depends on the type of hormone therapy you undergo:
- Removal of both testicles – erectile dysfunction is usually permanent.
- Hormone therapy – erectile dysfunction lasts for as long as hormone therapy is given. It can take 3–12 months after hormone therapy is stopped to regain erectile function. If erectile function does not come back on its own, treatments are available.
Your ability to have an erection depends on your sexual function before treatment, age and overall health.
What you can do…
- After your treatment, your doctor will prescribe medication that will allow you to regain your erectile capacity and a satisfying sex life.
- Treatments include oral drugs such as tadalafil, sildenafil, vardenafil; the MUSE pellet; penile injections; vacuum pumps; or surgical penile implants.
To know more about erectile dysfunction, take a look at our Side effects section.
Hot flashes
Although we tend to associate this inconvenience with women, hot flashes occur in about 50–80% of men who undergo hormone therapy. Hot flashes are a sudden feeling of unbearable heat that lasts for several minutes. It should be noted that hot flashes and fatigue tend to fade with time.
What you can do…
- Wear clothes that let your skin breathe (silk or cotton).
- Wear several layers of clothing that you can take off when you get too hot.
- Make sure that you have good air circulation in your home by opening windows and using fans.
- Drink fluids to stay hydrated—preferably cold, non-alcoholic, caffeine-free drinks.
- If you sweat a lot in bed, put towels on your mattress and pillows.
- Try taking a warm bath or shower instead of hot.
- Talk to your doctor about your hot flashes if they are unbearable—there are other treatments that can help.
Weight gain and muscle loss
Weight gain and muscle loss are common side effects of hormone therapy for prostate cancer. An increase in fatty tissues causes weight gain and loss of muscle tissues causes decreased strength.
What you can do…
- Diet and exercise help to reduce weight gain and muscle loss.
- You can also consult a nutritionist and kinesiologist (physical activity specialist) for additional support. Talk to your doctor, your nurse, or the social worker at your CLSC.
Loss of bone density (osteoporosis)
Osteoporosis is a long-term side effect that can occur with some hormonal drugs (LHRH). A bone mineral density test will determine your level of risk.
What you can do…
- Diet and exercise can help slow or prevent osteoporosis.
- Your doctor may prescribe products or medications to prevent or treat this complication: calcium, vitamin D, or other drugs such as bisphosphonates—if age or the effects of hormone therapy have made bones very fragile.
Changes in male characteristics
Hormone therapy decreases the size of your testicles. Men who took LHRH agonists noticed that their scrotum decreased in volume with time. In fact, the testes eventually atrophy after they stop functioning.
Breast swelling or tenderness
Breast swelling in men is called gynecomastia. This is a common side effect of hormone therapy for prostate cancer, particularly when an anti‑androgen, such as bicalutamide, is administered orally.
What you can do…
- Estrogen treatment and preventative breast radiation reduce the risk of breast tenderness and gynecomastia.
Fatigue
Fatigue causes a person to feel more tired than usual and can interfere with daily activities and sleep. Fatigue may improve with time, but it can also continue long after hormone treatment is completed. Physical activity can help you cope with fatigue.
What you can do…
- Exercise can help you cope with fatigue. To know more about managing fatigue, take a look at our Side effects
Depression
Hormone therapy for prostate cancer can sometimes cause depression and changes in emotional stability.
What you can do…
- Depression can be treated with antidepressants. To learn more about depression and how to recognize signs, take a look at our Side effects section
Anemia
Hormone therapy can cause anemia in some men. When the red blood cell count or hemoglobin level is slow, the body’s tissues don’t get enough oxygen. This causes fatigue and shortness of breath.
What you can do…
- Iron supplements can be taken orally as tablets or intravenously, depending on tolerance and circumstances.
- Iron levels cannot be increased through diet when iron deficiency is the result of unbearable pain.
Increased risk of cardiovascular disease
Hormone therapy causes weight gain, decreases your ability to exercise, and increases the level of lipids and glucose in your blood.
There are now two fact sheets, one for you as a patient and one for your family doctor. You should download and print them. If you do not have a printer, contact us at 1-855-899-2873. We will take care of mailing you a copy.
Fact sheet for you (blue) and for your family doctor (purple)

 What you can do…
What you can do…
- It is important to monitor your risk of heart disease and try to prevent or correct them as much as possible.
- The effects of your weight gain and muscle loss can be mitigated with diet and exercise.
Increased risk of developing a metabolic syndrome
Hormone therapy causes a decrease in cellular sensitivity to insulin. It also causes an increase in fatty tissues and a loss of muscle mass. These effects increase the risk of diabetes, dyslipidemia (e.g. increased cholesterol), obesity, and hypertension in men who undergo hormone therapy.
What you can do…
- The effects of your weight gain and muscle loss can be mitigated with diet and exercise.
- Download and print the hormone therapy fact sheet for patients. If you do not have a printer, contact us at 1 855 899-2873.
Tumour flare reaction
When first taken, LHRH agonists cause a temporary increase in testosterone levels that typically lasts for about a week. This hike which temporarily aggravates your symptoms is known as a tumour flare reaction. During the flare reaction, you may have urinary difficulties or bone pain.
What you can do…
- Your doctor may prescribe anti-androgens taken orally as a pill or liquid. Anti-androgens block the actions of androgens (male sex hormones) for a period of time to reduce flare symptoms.
Orchiectomy-related side effects
Surgical castration causes very few complications. Ordinarily, post-operative pain, scrotal swelling, and wound bleeding are minimal. As with any surgery, the scar can get infected. This infection will then be treated with antibiotics.
This surgery results in permanent side effects including erectile dysfunction and a decrease in sexual desire caused by low testosterone levels.
Suggestions and advice
 Give yourself time
Give yourself time
- There is a lot of information to retain. Don’t try to learn it all in one day.
- You will have questions. Write them down and bring them with you to your next appointment.
- Your body needs time to recover during treatment.
A healthy lifestyle will help you feel better
- Eat healthy
- Sleep a lot
- Do activities that you enjoy and that relax you
- Socialize
Accept help from others, they want what is best for you
- Practical help
- Emotional support
- Delegate tasks if you need to
- Do not be embarrassed to ask for help
Spend time with others and give them your attention
- Your friends and family also need comfort
- Keep a good line of communication open
- Resolve problems when they happen
Pursuing normal activities during treatment
Some men can continue to go to work and participate in their regular hobbies and activities while undergoing hormone therapy. Others have found that they tire easily and need more rest. Take a nap when you need one.
Visit our Living with cancer section for more information.
Questions to my doctor
Here is a list of questions about hormone therapy for you to ask your doctor and healthcare team.
Read more…
- What type of hormone therapy is used for this cancer?
- How is hormone therapy given? How often? Over what period of time?
- Does hormone therapy require a hospital stay? If so, for how long?
- What are the chances it will be successful? When will we know?
- What tests are done during hormone therapy?
- What are possible side effects of hormone therapy? When would they start? How long do they usually last?
- What side effects should I report right away? Who do I call?
- Are there special things that I should or should not do during and after hormone therapy?
- Will there be other treatments after hormone therapy? If so, what kind?
- When are follow-up visits scheduled? Who is responsible for follow-up after hormone therapy?
We are here for you
You have questions or concerns? Don’t hesitate. Contact us at 1-855-899-2873 to discuss with one of our nurses specialized in uro-oncology. They are there to listen, support and answer your questions, and those of your family or your loved ones. It’s simple and free, like all of our other services.
Also take the time to visit each of our pages on this website, as well as our YouTube channel, in order to get familiar with the disease, our expert lectures, our section on available resources, the support that is offered to you, our events and ways to get involved to advance the cause.
Staying Informed
Pages that might interest you
Want to know more? Just click on one of the links below.
The latest PROCURE news that might interest you
Every week we publish a blog article. Here are some we have chosen for you.
- Did you say prostate cancer?
- I want to postpone my treatment… Is that wise?
- I have several treatment options… Which one to choose?
The medical content and editorial team at PROCURE
Our team is composed of urologists, and nurses certified in uro-oncology with a deep knowledge of prostate cancer and other diseases related to the genitourinary system. Meet our staff by clicking here.
Sources and references
- Prostate Cancer – Understand the disease and its treatments; Fred Saad, MD, FRCSC and Michael McCormack, MD, FRCSC, 4th et 5th editions
- Canadian Cancer Society
- Prostate Cancer Foundation-PCF.org
- National Cancer Institute-USA
- American Cancer Society
- Memorial Sloan Kettering Cancer Center
- Prostate Cancer UK
Last medical and editorial review: April 2023
Written by PROCURE. © All rights reserved