Radiation therapy
Overview
 Radiation therapy is one of the main treatment options for men with prostate cancer. Technological developments now make it possible to destroy cancer cells while conserving neighbouring organs as much as possible. Radiation therapy can use high-intensity x-rays from a device or radioactive implants inserted into the prostate to kill cancer cells. It is used to potentially cure the cancer or to relieve pain or other symptoms (palliative care).
Radiation therapy is one of the main treatment options for men with prostate cancer. Technological developments now make it possible to destroy cancer cells while conserving neighbouring organs as much as possible. Radiation therapy can use high-intensity x-rays from a device or radioactive implants inserted into the prostate to kill cancer cells. It is used to potentially cure the cancer or to relieve pain or other symptoms (palliative care).
Why and for whom
Radiotherapy uses high-energy rays or particles to destroy cancer cells. Radiation can be used for prostate cancer:
- as the primary treatment to destroy cancer cells.
- after surgery to destroy cancer cells left behind and to reduce the risk of recurrence (adjuvant radiation therapy).
- after surgery if the cancer recurs in the area where the prostate gland was (salvage radiation therapy).
- to relieve pain or manage symptoms of advanced prostate cancer (palliative radiation therapy).
The amount of radiation given during treatment, as well as when and how it is given, is different for each person.
Types of radiation therapy
External beam radiation therapy
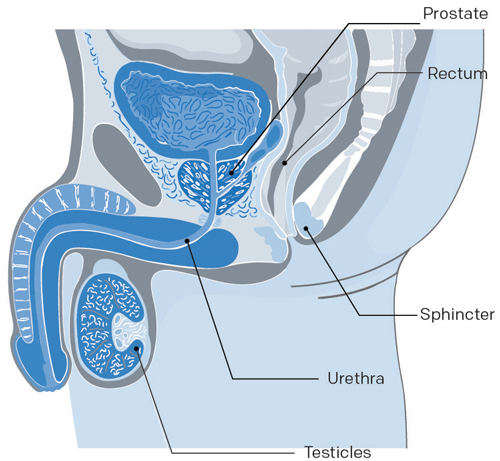
X-rays are emitted by a particle accelerator, whose beam, directed at the patient’s prostate, passes through the skin to destroy tumor cells. Depending on the case, radiotherapy can also be used to treat the affected lymph nodes. This treatment is painless.
Brachytherapy
Brachytherapy is internal radiation therapy. For this treatment, a radioactive material (radioactive isotope) is implanted directly into the prostate. The radiation destroys cancer cells over time. Brachytherapy is administered in two ways:
- High dose rate brachytherapy: Involves temporarily inserting a radioactive substance directly into the prostate using catheters connected to a radiation source. For cancers at a high risk of progression, this type of brachytherapy can be used in conjunction with external radiotherapy.
- Low dose rate brachytherapy: Radioative grains are permanently implanted in the prostate. This is generally a treatment option for relatively early stage cancers that are slow-growing and thus at a low risk of progression. It can also be an option for intermediate-risk cancers that meet a specific criteria.
Systemic radiation therapy
Systemic radiation therapy is a type of radiation therapy in which radioactive material travels through the bloodstream to reach cells all over the body.
Radium RA 223 dichloride (Xofigo) is a systemic radiation therapy drug, which may be used for castrate-resistant prostate cancer that causes pain and has spread only to the bone.
Is it for you
 Maybe
Maybe
External beam radiation therapy is used to treat prostate cancer using high intensity radiation beams. More precisely, it is the emission of radiation from an external source directed at the tumour and some of the normal surrounding tissue.
This treatment destroys cancer cells and prevents them from dividing and growing.
The benefits of ionizing radiation are not immediate but gradual as they depend on the cumulative effect of treatment sessions. Since cellular death continues for several months after radiation therapy has been completed, it is often necessary to wait a few months after starting treatment to assess the results.
Sources of external beam radiation therapy are X-rays and gamma rays, electron, proton, and neutron particles.
Modalities
Since radiation therapy also reaches healthy cells, radiation oncologists generally divide the treatment into small doses administered 5 times a week.
With this type of treatment schedule, healthy cells have time to heal over the weekend since cancer cells do not regenerate as easily as healthy cells.
The treatment itself takes about ten minutes. But you could probably spend an hour every day at the hospital in preparation for your treatment. You will not need to stay in the hospital overnight. The full treatment program can take 3-8 weeks.
External beam radiation therapy…
- does not hurt
- does not make the person radioactive
- cannot be seen, felt, or smelled
- does not require hospitalization or anesthesia
This treatment can lead to recovery if your cancer does not spread to other parts of your body.
Who can undergo external radiation therapy?
- Radiation therapy is for men with prostate cancer of all stages and risks of progression. It can be used as the sole treatment or in conjunction with hormone therapy.
- Men who are not good candidates for surgery because of other health problems or their age.
- Men in whom the cancer has not been completely eliminated or in whom the cancer has reappeared after surgery.
- Men whose cancer has spread beyond the prostate and into the surrounding tissues. The treatment is combined with hormone therapy before and after radiation therapy. This treatment can also be offered to men who have few metastases.
- Men whose cancer cells have spread to the bones, to help reduce the size of the tumor or to ease the pain caused by bone metastases.
Reasons for choosing radiation therapy
For many men with localized prostate cancer, radiation provides an effective treatment without the risks and recovery time associated with surgery.
For men with a 7–10 year life expectancy, radiation therapy appears to have the same success rate as surgery.
Types of external radiation therapy
Radiation therapy has become much more precise over the past few years. The standard treatment now used in most radiology departments is known as “3‑D conformal radiation therapy” or “intensity‑modulated radiation therapy (IMRT)”.
Powerful computers and tomographic scans (CT or CAT scans) generate a more exact, three-dimensional picture of the prostate. These images enable increased precision when administering radiation which maximizes the impact on cancer cells. This in turn reduces the negative effects of radiation exposure on healthy surrounding tissues which then reduces the risk of side effects.
Advantages and limitations
 Advantages of radiation therapy
Advantages of radiation therapy
- If your cancer is localized or locally advanced, radiation could get rid of it completely.
- Radiation therapy may be an option if you are not fit or well enough for surgery.
- Many men are able to continue their normal activities during treatment.
- You avoid surgery, general anesthesia, and all associated complications.
- Sessions are short, painless and do not necessitate a hospital stay.
Limitations of radiation therapy
- Traveling 5 days a week for several weeks. This can be inconvenient depending on the distance and method of transportation.
- We cannot know the full nature and extent of your tumor as we do with surgery.
- Failures can only very rarely be treated through surgery (exceptions). Radiation therapy may have damaged your prostate and surrounding tissues, making it more difficult to remove the prostate and increasing the risk of side effects.
- A significant decrease in your ejaculate and loss of fertility if you want children.
Risks and complications
Radiation therapy damages cancer cells. Healthy cells in the treatment area can also be damaged, even if precautions are taking to protect normal tissue as much as possible. Side effects are caused by damage to healthy cells. However, external beam radiation therapy does not affect all men in the same way.
Short term
Short-term risks and complications can appear several weeks after starting radiation therapy and will slowly go away within a year of finishing treatment. You may have one of the following side effects:
- Fatigue: lack of energy, weight loss, or changes in your appetite.
- Gastro-intestinal or rectal problems: diarrhea, stomach cramps, painful bowel movements, rectal bleeding, anal irritation.
- Urinary problems: burning feeling during urination, frequent urination, difficulty urinating, blood in the urine, and urinary incontinence (leakage).
- Skin reactions: redness, itching, dry skin, and hair loss only in the area being treated with radiation. You will not lose the hair on your head or elsewhere.
Medium–long term
Some side effects, however, may continue after treatment is over because it takes time for healthy cells to recover from the effects of radiation therapy. Late side effects can occur months or years after treatment. Side effects may vary:
- Scar tissue in the urinary passage slows urinary flow
- Permanent changes to the frequency of your bowel movements
- Blood in your stool or urine
- Significant decrease in fluid ejaculation and loss of fertility
- Erectile dysfunction
It is important to report any side effects to your radiotherapy team. Most side effects can be alleviated with medication, dietary changes, or other measures.
What to expect
 Your doctor has recommended radiation therapy to treat your prostate cancer. This section explains the treatment and precautions to take so that everything goes as smoothly as possible.
Your doctor has recommended radiation therapy to treat your prostate cancer. This section explains the treatment and precautions to take so that everything goes as smoothly as possible.
Terminology
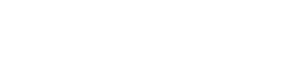
To familiarize you with medical language, here is a brief description of structures that make up the male reproductive system.
Bladder: The muscular sac-like organ in which urine is collected and stored in the body.
Prostate: The gland located just below the bladder that surrounds the urethra. It secretes fluids that mix with sperm cells to form semen.
Rectum: The terminal section of the large intestine.
Sphincter: The muscle located at the opening between the bladder and the prostate. The sphincter prevents urine from leaking out of the bladder—controlling urinary continence.
Seminal vesicles: Small pouches alongside the prostate that store sperm produced by the prostate.
Urethra: The tube that carries urine from the bladder and sperm secreted by the genital glands out through the penis.
Testicles: The two glands located inside the scrotum that form sperm cells and produce testosterone (male hormone).
Modalities for external radiotherapy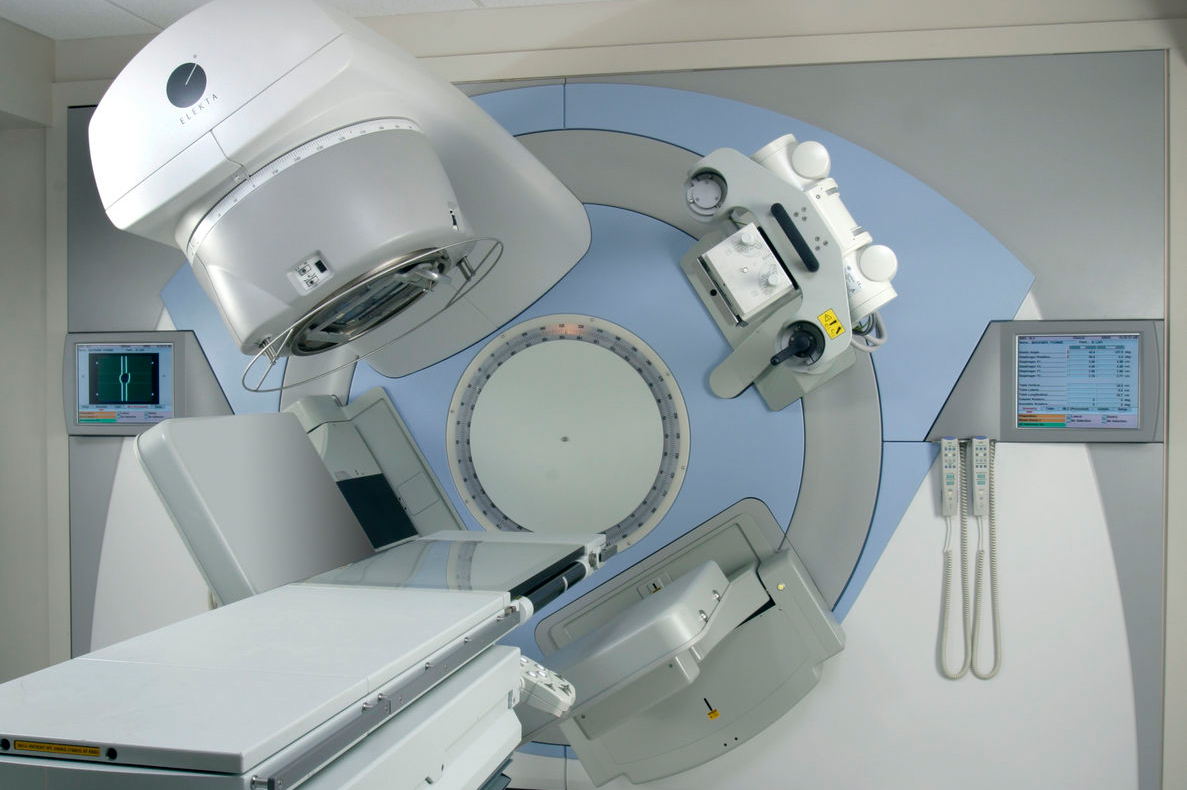
Pre-treatment visits
Shortly before starting your treatment, you will meet with your medical team in order to prepare you for it. Normally, three visits are planned: one with your radiation oncologist (or more if necessary), one for the implantation of gold or platinum grains and one for simulation or to plan your scan.
Simulation
The simulation is a planning session that happens before the first external beam radiation therapy session. It ensures that the radiation will be directed to exactly the same spot every session.
Duration of the intervention
Treatments usually take 4 to 8 weeks. It is possible that your treatment is shorter, if you are part of a research group or if you also receive a high dose rate brachytherapy (another type of radiation therapy). If this is the case, you will receive a document with further explanations.
Getting ready
 Before your radiation therapy
Before your radiation therapy
Be active
It is important to move to stay healthy, even if you have prostate cancer. Consequently, if you’re already practicing a regular activity, you should continue doing it. If this is not the case, it’s never too late to add exercising to your daily routine; even if it’s at a lower intensity.
Even taking a short 15–30 minute walk can be beneficial.
Try to stop smoking
Even if it’s stressful, it is recommended that you stop smoking 6 weeks before your surgery in order to reduce the risks of lung, healing, and infection problems. If needed, your doctor may prescribe medication to help you.
Reduce your alcohol consumption
Alcohol can also interact with medication. This is why it is recommended to reduce its consumption and not drink in the 24 hours before surgery.
Adopt good eating habits
A healthy and balanced diet will help you to recover quickly after your treatments. The energy, proteins, vitamins, and minerals that you get from your food can also help fight against these infections and help contribute to your healing.
Basic advice for you
- Have 3 meals a day and snacks when you need them.
- Eat food from all four of Canada’s Food Guide (low-fat dairy products, fruits and vegetables, grain products, lean meat, skinless poultry, fish, and other alternatives) in order to ensure you get your daily intake of various nutrients.
- Have at least one meal a day that consists of lean meat, skinless poultry, or fish in order to ensure you get your daily intake of various nutrients.
- Fruits and vegetables are an excellent and important source of vitamins and minerals.
- Drink enough water—at least 1 500 mL a day or 6–8 glasses.
In cases of diarrhea, patients are often seen by the nutritionist to make dietary adjustments as needed.
Your medication
Ask your doctor what to do before you stop taking your medication.
Avoid natural products
If needed, discuss it with your radio-oncologist first.
Planning your sick leave together with your employer
If you need to receive your treatment in another region, you will have no choice but to announce it to your employer. Planning your sick leave and your return to work is important for your recovery; it will clear your conscience. It will be necessary to address the subject as early as possible if you work.
If you have private insurance, talk to your insurer or your company’s Human Resources to manage your absence and minimize your stress.
Arrange transportation
If you live in an urban area, close to the hospital centre where the procedure will take place, getting there will not be a problem. However, distance and repeat visits can be problematic—transportation and accommodation support becomes necessary for the success of the whole treatment.
Are your treatments far from home?
If necessary, contact the Quebec Cancer Foundation for your accommodation. It offers affordable, comfortable, and safe accommodation near major radio-oncology centers. Their hotels in Montreal, Gatineau, Sherbrooke and Trois-Rivières will welcome you and a close friend for the duration of your treatments.
The hospital where your treatment takes place is responsible for helping you with your travel and accommodation needs.
The Ministry of Health And Social Services has revised its Déplacement des usagers Policy and forwarded it to the Directors of all Health and Social Services Institutions and to the Presidents or CEOs of all Health and Social Service Agencies.
In its introduction, the document states: Travel for a user residing in Quebec requiring transportation to an institution in the Health and Social Services network is not covered by the Régie de l’assurance maladie du Québec. Initially, all transportation to an affiliated Institution was the responsibility of the person being transported unless eligible for the free government program.
In general, it is the job of the social worker assigned by the referent Institution to aid you in finding transportation or accommodation and in providing you with the rules and details of the transportation program that are applicable to your case.
Before starting your treatment
 First visit: Meeting with radiation oncologist
First visit: Meeting with radiation oncologist
Before starting radiation therapy, you will first meet with the radio-oncologist who will explain the principle, objectives, and techniques to be used. You will also be informed of possible adverse reactions and the solutions that exist to prevent or limit them. Feel free to ask any questions you may have about this treatment.
Second visit: Implanting gold or platinum pellets
In some treatment centres, 3–4 gold or platinum pellets are implanted during the radiotherapy treatment to increase the precision of the localization. The pellets allow the radio-oncologist to see the prostate, which can slightly shift between sessions, more clearly and aim the beam with precision.
During your first visit, the medical team will implant 3–4 pellets into your prostate with the help of an ultrasound machine inserted into your rectum. This procedure is very similar to that used during your biopsy.
These pellets are reference markers that will permanently stay in your prostate but will have no side effects.
- Antibiotics will be prescribed to prevent infection. You will need to take them the night before your visit, the day of your visit, and the day after your visit.
- In preparation, you should also perform a Fleet enema the morning of the visit.
Third visit: Simulating a radiation therapy session
The CT simulation is a planning session that happens before the first external beam radiation therapy session. The scans ensure that the radiation will be directed to exactly the same spot every session.
Treatment plan: During the second visit, the medical team will examine the inside of your body using an imaging machine known as a CT scanner. This exam, called a CT scan or a computerized axial tomography (CAT scan), precisely defines the area of your body that will be treated while steering clear, as much as possible, of parts that are not sick. This is what we call a “treatment plan”.
For this visit, and in all future treatments, your bladder should be full. You will be given instructions to guide you.
Positioning: A technologist will determine exactly what position you should be in for all of your treatments. If necessary, the radiotherapy technologists may use special equipment to help keep you in the desired position. Immobilizers are specially designed to fit the shape of a person.
The prostate can shift slightly inside the pelvis depending on the volume of fecal matter or urine contained in the bladder and rectum. Your healthcare team will endeavour to reduce prostate movement by asking you to follow the same daily schedule for filling your bladder and clearing your rectum. If everything meets the standards, the plan will be approved and your treatment can start.
Skin markings: The technologist will then mark your skin with small tattooed dots that will serve as reference points throughout the treatment.
Verification and first treatment
You will first meet with the radiation oncology technologists to discuss your treatment steps. Do not hesitate to ask them YOUR questions.
This final visit will be to check if the treatment area is consistent with the treatment plan. You will need to get into the same position that you will be in for all your treatments—you will have the required accessories to keep you in position.
Then you will receive your first treatment immediately.
During treatment
 During your radiation therapy
During your radiation therapy
You will always be in the same position for each treatment.
During each session, technologists will make sure that everything is working well from a technical standpoint. They will also take pictures to locate the prostate through the platinum pellets. After checking that you’re in the right position, they leave the room. An intercom and cameras will keep you in contact with them—they can see you, hear you, and speak to you.
After your treatment, a technologist will give you the date and time of your next appointment.
During the treatment, you will have regular appointments with your radiation oncologist to monitor side effects and check on your progress.
Will I feel pain?
You will feel no pain during the treatment. However, you will probably develop side effects after several treatments.
Safety measures
External beam radiation therapy does not make a person radioactive. It is not dangerous to be around people, including children, right after treatment.
At home
 Instructions
Instructions
Take care of your skin
- Wash the radiation-treated areas with mild unscented soap, without lanolin and of a neutral pH. If necessary, consult a pharmacist.
- If needed, your doctor may prescribe a cream to use during treatment.
- Do not use any product on the treated skin without first talking to your doctor.
- Wear loose clothing to reduce irritating treated areas. Choose cotton or natural fabrics.
- Cover the treated area to protect it from the sun.
- Do not apply heat or cold directly to the treated area.
- Do not wash off the marks the team draws on your skin
Avoid foods that increase intestinal activity
- Whole-grain bread, prunes, dried fruits, cucumbers, corn, leeks, fermented cheese (brie, Oka), legumes, a lot of juice, ice cream, etc.
- Reduce your consumption of coffee and milk. A nutritionist will answer YOUR questions.
- Drink lots of water
Activities during treatment
Some people can continue to work and perform their regular recreational activities while undergoing radiation therapy. Others note that they tire easily and need to rest more. Take naps when you need them.
Physical contact and sexual activity are safe after external beam radiation therapy. It is possible that after treatment is over, some people need to take better care of their skin for a while.
Medical follow-up
 The importance of follow-ups
The importance of follow-ups
Medical certificate
If you need a medical certificate, don’t forget to ask your radiation oncologist.
Results
As with radical prostatectomies, it is impossible to estimate the average success rate of radiation therapy.
- Success will vary from person to person because of individual differences in the grade of the tumour, the degree to which the cancer has spread, and the PSA level before treatment.
- The less severe these three factors are, the better the patient’s chances are of being in the clear.
PSA tests
Every three to six months, a digital rectal exam is performed and your prostate‑specific antigen (PSA) level is measured since this test is the best predictor for the risk of recurrence of prostate cancer.
Your PSA level
With radiation therapy, PSA levels will generally not fall all the way down to 0 ng/mL because there are still normal prostatic cells left. Your PSA levels should begin to drop in the months following the start of treatment and may continue to drop for as long as a year after treatment ends. In general, after dropping, it remains stable.
At each medical appointment, your urologist will check 3 parameters:
- if the PSA level is higher
- how much time has it been since the operation and
- how much time does it take this level to double (velocity)
Recurrence
If the PSA level starts to climb, the doctor will monitor how much time it takes to double. The shorter these periods are, the greater the risk of recurrence and the more aggressive the recurrence will be. For example, a PSA level that starts to increase eight months after the operation and that doubles in six months is much more worrisome than a PSA level that starts to climb three years after the radiation treatment and takes a year to double.
If necessary, hormone therapy may be prescribed.
Remission
You will be monitored for at least five years after your radiation therapy treatment. If everything goes well, after seven to ten years without recurrence, the risk of recurrence is very low.
Side effects
 Advances in radiation techniques have made the onset of later side effects both less frequent and less severe. However, some symptioms can appear several months or even years after treatment has ended. The most common problems associated with brachytherapy are urinary, gastro-intestinal, and erectile functional problems.
Advances in radiation techniques have made the onset of later side effects both less frequent and less severe. However, some symptioms can appear several months or even years after treatment has ended. The most common problems associated with brachytherapy are urinary, gastro-intestinal, and erectile functional problems.
Intestinal and urinary functions
Sometimes intestinal and urinary functions do not return to normal after treatment is complete. This happens to 5–10% of men.
- Some medications (such as cortisone that reduces rectal inflammation) and muscle relaxants can sometimes help alleviate these symptoms.
- Make an appointment with a nutritionist or dietician for your intestinal problems.
- Discuss your urinary problems with your doctor. Urinary problems can often be corrected with medication or a procedure
Blood in your urine or stool
- The presence of blood in the urine (microscopic haematuria) is sometimes observed. If you see blood in your urine, tell your urologist.
- You may also notice blood in your stool. Most often, this is a problem that will disappear quickly at the end of your treatment. However, you should talk to your doctor who may want a consultation with a specialist who will be able to assess the bleeding.
To know more about urinary and intestinal problems, check out our section on side effects.
Erectile Fonction
Erectile problems
The percentage risk of erectile dysfunction varies for each patient. However, unlike other side effects, erectile dysfunction appears gradually several months or even years after treatment but does not affect one’s enjoyment.
- As cellular death happens gradually, you will still be able to have an erection at first, but will slowly lose the ability with time.
- Your erectile capacity depends on your sexual function before treatment, your age, your general state of health
- Your erectile function will be affected more if your radiation therapy is combined with hormone therapy since you will lose your libido.
To learn more about incontinence or erectile dysfunction, take a look at our section on side effects.
Erectile dysfunction treatments
When you start experiencing erectile dysfunction, your doctor will prescribe medication that will help you regain your erectile capacity and a satisfying sex life.
Treatments include oral medication such as tadalafil, sildenafil, and vardenafil; the MUSE pellet; penile injections; vacuum pumps; or surgical penile implants.
Your libido and orgasms
Your libido and ability to have orgasms remain intact. It should be stressed that your orgasm (feelings of enjoyment) is not affected since it is controlled by other nerves located far from your prostate. Your sex drive (libido) will also remain intact, unless you undergo hormone therapy.
Your ejaculations and loss of fertility
Radiation therapy “dries out” your prostate, so you can expect a significant decrease in ejaculate. Seminal liquid, which you will no longer produce, keeps your sperm cells healthy, which is why you usually become infertile.
If you want to have children, you will need to call a sperm bank. Discuss it with both your doctor and partner.
Suggestions and advice
 Give yourself time
Give yourself time
- There is a lot of information to retain. Don’t try to learn it all in one day.
- You will have questions. Write them down and bring them with you to your next appointment.
- Your body needs time to recover during treatment.
A healthy lifestyle will help you feel better
- Eat healthily
- Sleep a lot
- Do activities that you enjoy and that relax you
- Socialize
Accept help from others, they want what is best for you
- Practical help
- Emotional support
- Delegate tasks if you need to
- Do not be embarrassed to ask for help
Spend time with others and give them your attention
- Your friends and family also need comfort
- Keep a good line of communication open
- Resolve problems when they happen
Questions to my doctor
Here is a list of questions about radiation therapy for you to ask your doctor and healthcare team.
Read more…
- What type of radiation therapy is used for this cancer?
- How is radiation therapy given? How often? Over what period of time?
- Does radiation therapy require a hospital stay? If so, for how long?
- What are the chances it will be successful? When will we know?
- What tests are done during radiation therapy?
- What are possible side effects of radiation therapy? When would they start? How long do they usually last?
- What side effects should I report right away? Who do I call?
- Are there special things that I should or should not do during and after radiation therapy?
- Will there be other treatments after radiation therapy? If so, what kind?
- When are follow-up visits scheduled? Who is responsible for follow-up after radiation therapy?
We are here for you
You have questions or concerns? Don’t hesitate. Contact us at 1-855-899-2873 to discuss with one of our nurses specialized in uro-oncology. They are there to listen, support and answer your questions, and those of your family or your loved ones. It’s simple and free, like all of our other services.
Also take the time to visit each of our pages on this website, as well as our YouTube channel, in order to get familiar with the disease, our expert lectures, our section on available resources, the support that is offered to you, our events and ways to get involved to advance the cause.
Staying Informed
Pages that might interest you
Want to know more? Just click on one of the links below.
The latest PROCURE news that might interest you
Every week we publish a blog article. Here are some we have chosen for you.
- Did you say prostate cancer?
- I want to postpone my treatment… Is that wise?
- I have several treatment options… Which one to choose?
The medical content and editorial team at PROCURE
Our team is composed of urologists, and nurses certified in uro-oncology with a deep knowledge of prostate cancer and other diseases related to the genitourinary system. Meet our staff by clicking here.
Sources and references
- Prostate Cancer – Understand the disease and its treatments; Fred Saad, MD, FRCSC and Michael McCormack, MD, FRCSC, 4th et 5th editions
- Canadian Cancer Society
- Prostate Cancer Foundation-PCF.org
- National Cancer Institute-USA
- American Cancer Society
- Memorial Sloan Kettering Cancer Center
- Prostate Cancer UK
Last medical and editorial review: September 2023
Written by PROCURE. © All rights reserved